Nephrons are the “functional units” of the kidney; they cleanse the blood of toxins and balance the constituents of the circulation to homeostatic set points through the processes of filtration, reabsorption, and secretion. The nephrons also function to control blood pressure (via production of renin), red blood cell production (via the hormone erythropoetin), and calcium absorption (via conversion of calcidiol into calcitriol, the active form of vitamin D).
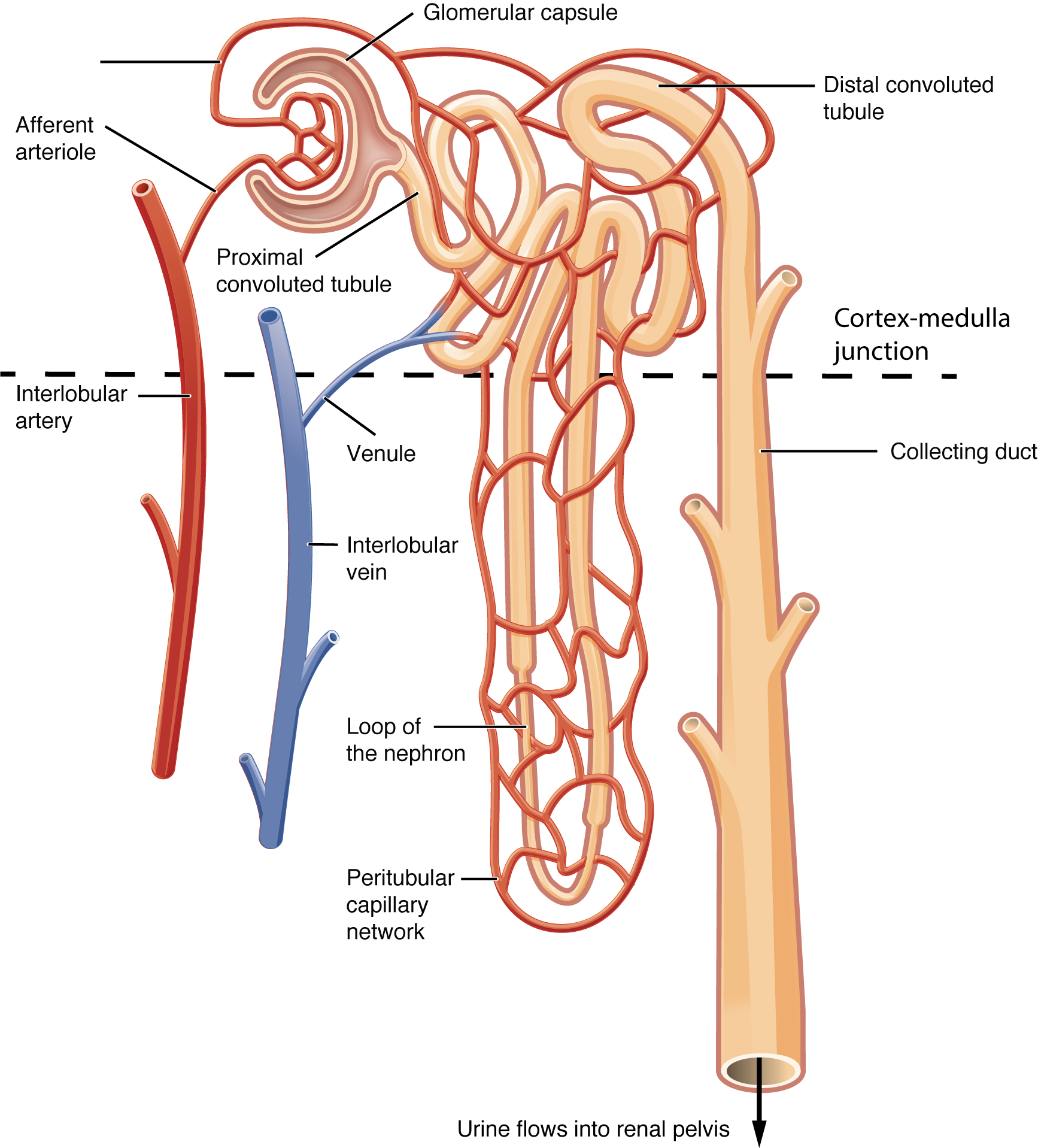
Each nephron consists of a blood supply and a specialized network of ducts called a tubule. For each nephron, an afferent arteriole feeds a high-pressure capillary bed called the glomerulus. Blood is filtered by the glomerulus to produce a fluid which is caught by the nephron tubule, called filtrate. The proximal end of the tubule that surrounds the glomerulus and catches the filtered fluid is the glomerular (Bowman’s) capsule. The glomerulus and glomerular capsule together form the renal corpuscle. Filtered fluid caught by the glomerular capsule (filtrate) travels through the rest of the tubule to the proximal convoluted tubule (PCT), loop of Henle and distal convoluted tubule (DCT), in this order, before exiting the nephron into common collecting ducts shared by many nephrons. Though all nephron glomeruli are in the cortex, some nephrons have short loops of Henle that do not dip far beyond the cortex. These nephrons are called cortical nephrons. About 15 percent of nephrons have very long loops of Henle that extend deep into the medulla and are called juxtamedullary nephrons.
Blood exits the glomerulus into the efferent arteriole (Figure 25.2.1). The efferent arteriole then forms a second capillary network around the tubule, called the peritubular capillaries. For juxtamedullary nephrons, the portion of the capillary that follows the loop of Henle deep into the medulla is called the vasa recta. As the glomerular filtrate progresses through the tubule, these capillary networks recover most of the solutes and water, and return them to the circulation. Since a capillary bed (the glomerulus) drains into a vessel that in turn forms a second capillary bed, this is another example of a portal system (also seen in hypothalamus-pituitary axis and hepatic portion of the digestive system).
Visit this link to view an interactive tutorial of the flow of blood through the kidney.
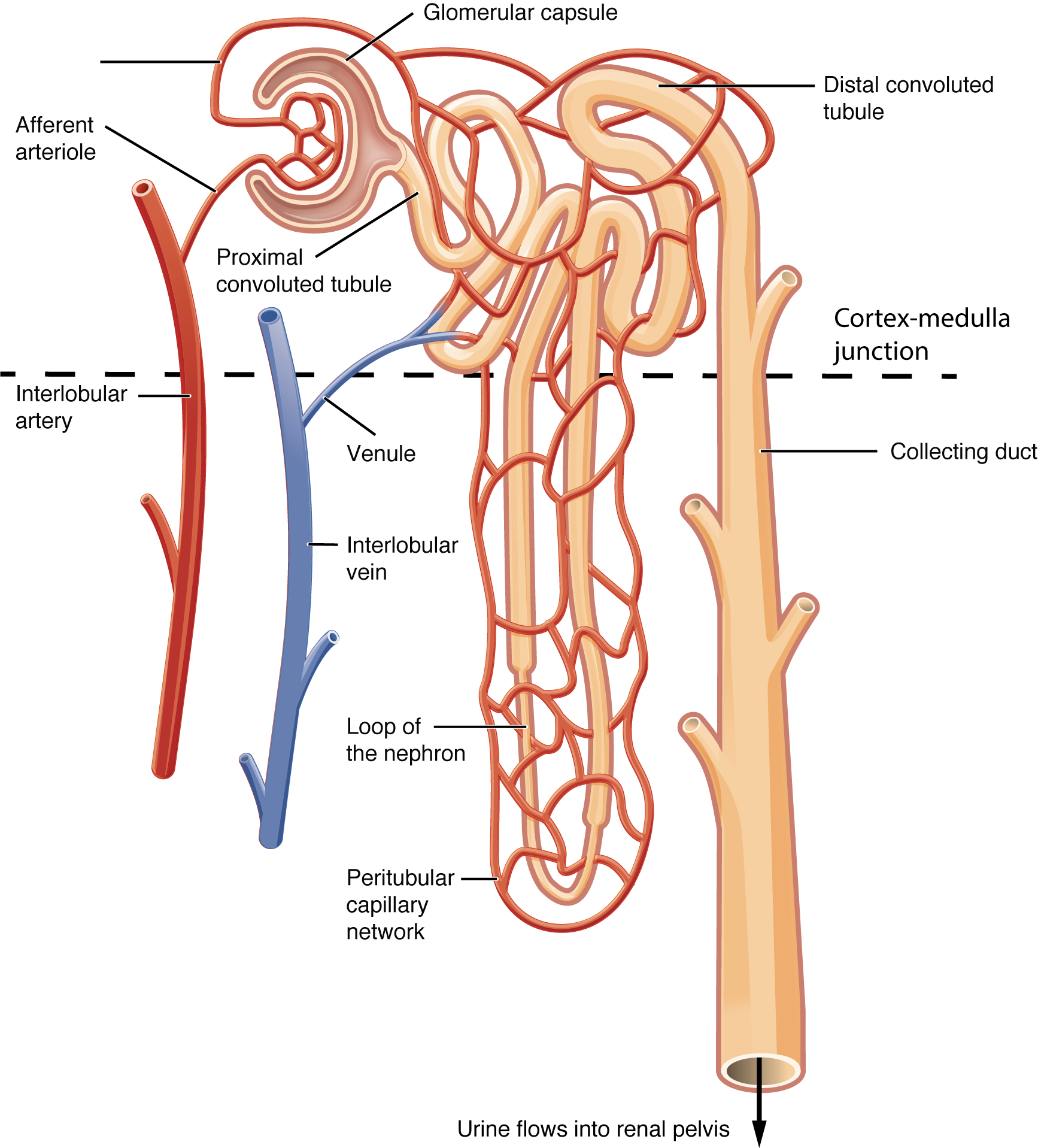
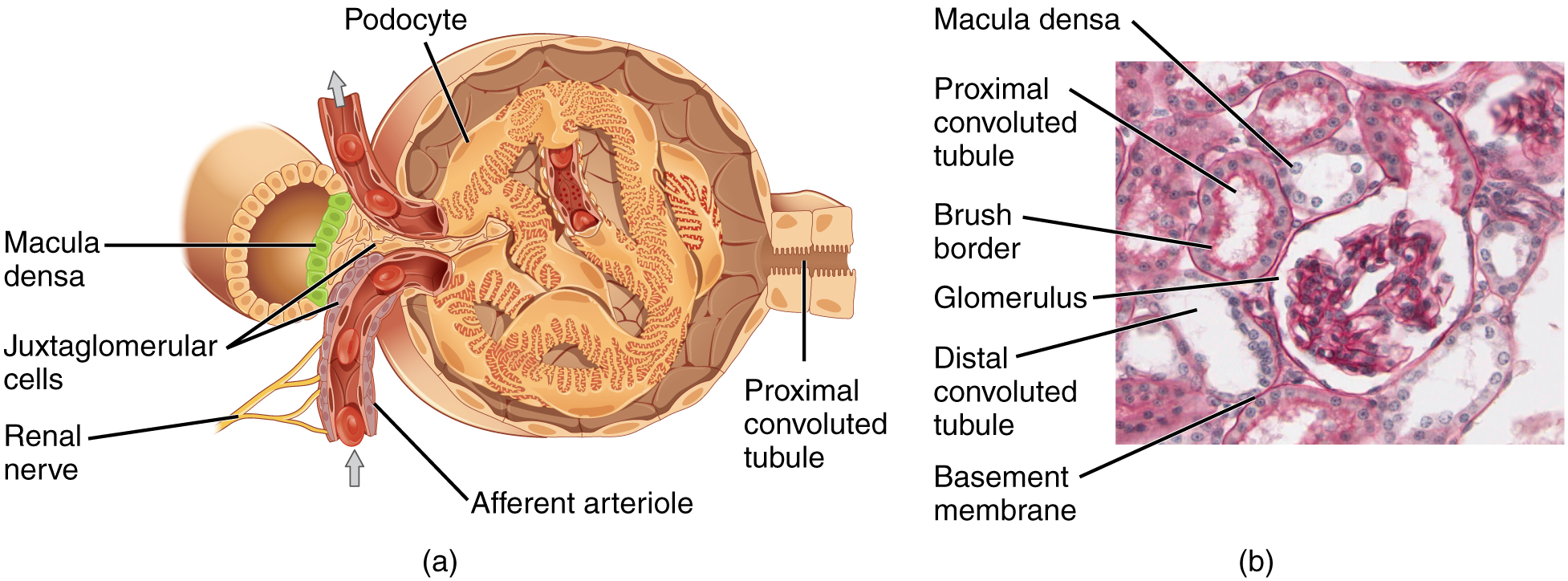
As discussed earlier, the renal corpuscle consists the glomerulus and the glomerular capsule. The glomerulus is a high pressured, fenestrated capillary with large holes (fenestrations) between the endothelial cells. The glomerular capsule captures the filtrate created by the glomerulus and directs this filtrate to the PCT. The outermost part of glomerular capsule is a simple squamous epithelium. It transitions over the glomerulus as uniquely shaped cells (podocytes) with finger-like arms (pedicels) that cover the glomerular capillaries (Figure 25.2.2). A thin basement membrane lies between the glomerular endothelium and the podocytes. The pedicels interdigitate to form filtration slits, leaving small gaps that form a sieve. As blood passes through the glomerulus, 10 to 20 percent of the plasma filters out of the fenestrations, through the basement membrane and between these sieve-like fingers to be captured by the glomerular capsule and funneled to the PCT. These features comprise the filtration membrane.
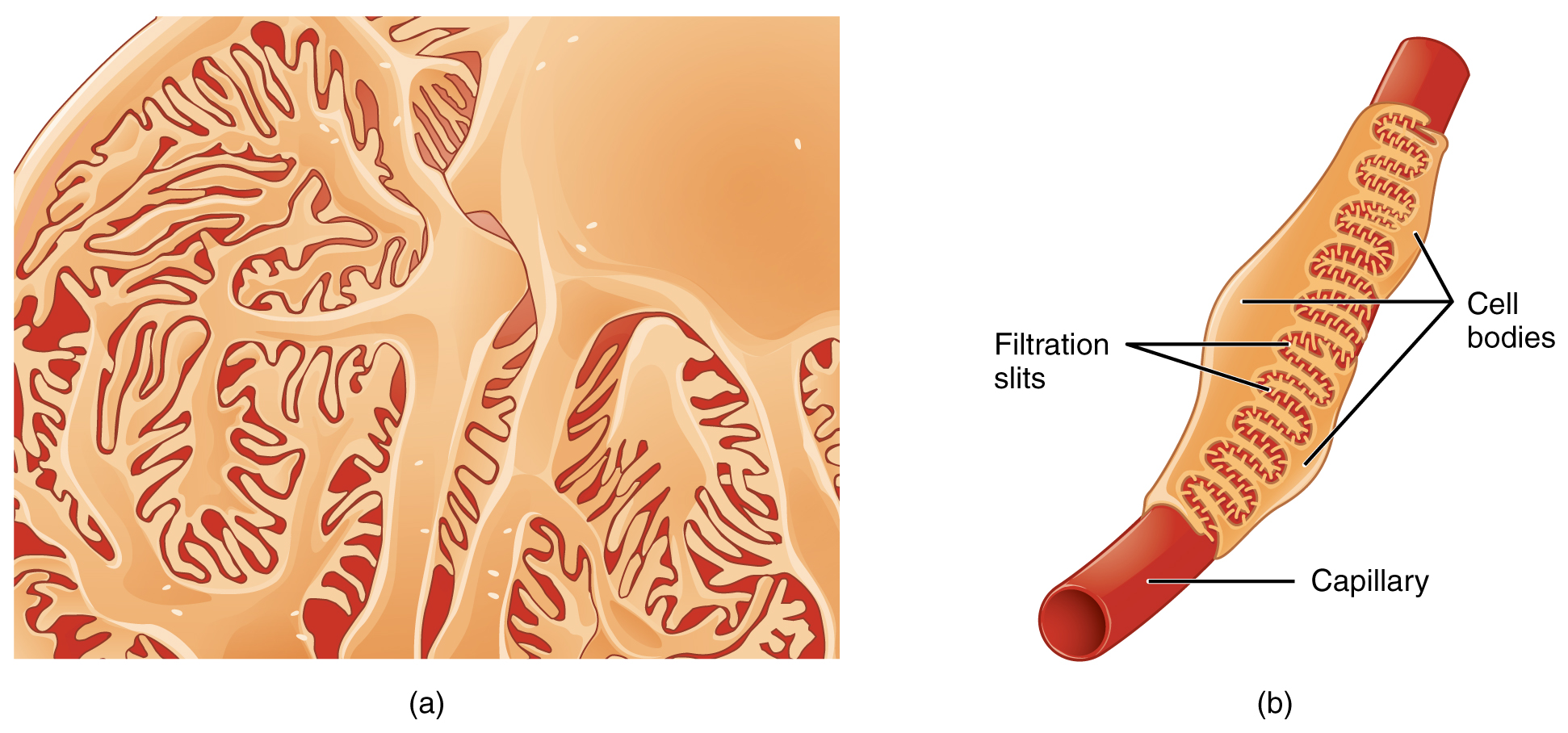
The filtration membrane prevents passage of blood cells, large proteins, and most negatively charged particles but allows most other constituents through. These substances cross readily if they are less than 4 nm in size and most pass freely up to 8 nm in size. Negatively charged particles have difficulty leaving the blood because the proteins associated with the filtration membrane are negatively charged, so they tend to repel negatively charged substances and allow positively charged substances to pass more readily. There are also mesangial cells in the filtration membrane that can contract to help regulate the rate of filtration of the glomerulus. The result is the creation of a filtrate that does not contain cells or large proteins, and has a slight predominance of positively charged substances.
Filtered fluid collected by Bowman’s capsule enters into the PCT. Simple cuboidal cells form this tubule with prominent microvilli on the luminal surface, forming a brush border. These microvilli create a large surface area to maximize the absorption and secretion of solutes in the filtrate (Na + , Cl – , glucose, etc.), the most essential function of this portion of the nephron. These cells actively transport ions across their membranes, so they possess a high concentration of mitochondria in order to produce sufficient ATP.
The descending and ascending portions of the loop of Henle (sometimes referred to as the nephron loop) are continuations of the same tubule. They run adjacent and parallel to each other after having made a hairpin turn at the deepest point of their descent. The descending loop of Henle consists of an initial short, thick portion and long, thin portion, whereas the ascending loop consists of an initial short, thin portion followed by a long, thick portion. The descending thick portion consists of simple cuboidal epithelium similar to that of the PCT. The descending and ascending thin portions consists of simple squamous epithelium. As you will see later, these are important differences, since different portions of the loop have different permeabilities for solutes and water. The ascending thick portion consists of simple cuboidal epithelium similar to the DCT.
The DCT, like the PCT, is formed by simple cuboidal epithelium, but it is shorter than the PCT. These cells are not as active as those in the PCT and there are fewer microvilli on the apical surface. However, these cells must also pump ions against their concentration gradient, so you will find of large numbers of mitochondria, although fewer than in the PCT.
The collecting ducts are continuous with the nephron but not technically part of it. In fact, each duct collects filtrate from several nephrons for final modification. Collecting ducts merge as they descend deeper in the medulla to form about 30 terminal ducts, which empty at a papilla. They are lined with simple cuboidal epithelium to facilitate water transport.
 of this image shows the cross section of the juxtaglomerular apparatus. The major parts are labeled." width="550" height="204" />
of this image shows the cross section of the juxtaglomerular apparatus. The major parts are labeled." width="550" height="204" />
Lying just outside Bowman’s capsule and the glomerulus is the juxtaglomerular apparatus (JGA) (Figure 25.2.4). At the juncture where the afferent and efferent arterioles enter and leave Bowman’s capsule, the initial part of the distal convoluted tubule (DCT) comes into direct contact with the arterioles, the structure that feeds the glomerulus. The wall of the DCT at that point forms a part of the JGA known as the macula densa. This cluster of cuboidal epithelial cells monitors the fluid composition of fluid flowing through the DCT. In response to the concentration of Na + in the fluid flowing past them, these cells release paracrine signals (ATP or adenosine). They also have a single, nonmotile cilium that responds to the rate of fluid movement in the tubule. The paracrine signals released in response to changes in flow rate and Na + concentration are adenosine triphosphate (ATP) and adenosine. A second function of the macula densa cells is to regulate renin release from the juxtaglomerular cells of the afferent arteriole. Renin is a protein that initiates the production of Angiotensin II, which acts as a powerful systemic vasoconstrictor and stimulates the release of the hormone aldosterone from the adrenal cortex. A second cell type in this apparatus is the juxtaglomerular (JG) cell, or granular cell. This is a modified, smooth muscle cell lining the afferent arteriole that can contract or relax in response to ATP or adenosine released by the macula densa. Such contraction and relaxation regulate blood flow to the glomerulus. Juxtaglomerular cells also produce renin which initiates a cascade of events to control systemic blood pressure, to be discussed later.
The functional unit of the kidney, the nephron, consists of the renal corpuscle, PCT, loop of Henle, and DCT. Cortical nephrons have short loops of Henle, whereas juxtamedullary nephrons have long loops of Henle extending into the medulla. About 15 percent of nephrons are juxtamedullary. The glomerulus is a capillary bed that filters blood principally based on particle size. The filtrate is captured by Bowman’s capsule and directed to the PCT. A filtration membrane is formed by the fused basement membranes of the podocytes and the capillary endothelial cells that they embrace. Contractile mesangial cells further perform a role in regulating the rate at which the blood is filtered. Specialized cells in the JGA produce paracrine signals to regulate blood flow and filtration rates of the glomerulus. Other JGA cells produce the enzyme renin, which plays a central role in blood pressure regulation. The filtrate enters the PCT where absorption and secretion of several substances occur. The descending and ascending limbs of the loop of Henle consist of thick and thin segments. Absorption and secretion continue in the DCT but to a lesser extent than in the PCT. Each collecting duct collects forming urine from several nephrons and functions to fine tune water recovery.
1. Which structures make up the renal corpuscle?
2. What are the major structures comprising the filtration membrane?
brush border formed by microvilli on the surface of certain cuboidal cells; in the kidney it is found in the PCT; increases surface area for absorption in the kidney calyces cup-like structures receiving urine from the collecting ducts where it passes on to the renal pelvis and ureter efferent arteriole arteriole carrying blood from the glomerulus to the capillary beds around the convoluted tubules and loop of Henle; portion of the portal system fenestrations small windows through a cell, allowing rapid filtration based on size; formed in such a way as to allow substances to cross through a cell without mixing with cell contents filtration slits formed by pedicels of podocytes; substances filter between the pedicels based on size filtrate a plasma-like liquid (lacking most proteins) formed by the glomerulus and modified through secretion and reabsorption before true urine is produced glomerulus tuft of capillaries surrounded by Bowman’s capsule; filters the blood based on size juxtaglomerular apparatus (JGA) located at the juncture of the DCT and the afferent and efferent arterioles of the glomerulus; plays a role in the regulation of renal blood flow and GFR juxtaglomerular cell modified smooth muscle cells of the afferent arteriole; secretes renin in response to a drop in blood pressure macula densa cells found in the part of the DCT forming the JGA; sense Na + concentration in the forming urine mesangial contractile cells found in the glomerulus; can contract or relax to regulate filtration rate nephrons functional units of the kidney that carry out all filtration and modification to produce urine; consist of renal corpuscles, proximal and distal convoluted tubules, and descending and ascending loops of Henle; drain into collecting ducts pedicels finger-like projections of podocytes surrounding glomerular capillaries; interdigitate to form a filtration membrane peritubular capillaries second capillary bed of the renal portal system; surround the proximal and distal convoluted tubules; associated with the vasa recta podocytes cells forming finger-like processes; form the visceral layer of Bowman’s capsule; pedicels of the podocytes interdigitate to form a filtration membrane renin enzyme produced by juxtaglomerular cells in response to decreased blood pressure or sympathetic nervous activity; catalyzes the conversion of angiotensinogen into angiotensin I
Answers for Critical Thinking Questions
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax, are licensed under CC BY except where otherwise noted.
Anatomy & Physiology Copyright © 2019 by Lindsay M. Biga, Staci Bronson, Sierra Dawson, Amy Harwell, Robin Hopkins, Joel Kaufmann, Mike LeMaster, Philip Matern, Katie Morrison-Graham, Kristen Oja, Devon Quick, Jon Runyeon, OSU OERU, and OpenStax is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License, except where otherwise noted.